|
Assembly Actions -
Lowercase Senate Actions - UPPERCASE |
|
|---|---|
| Apr 28, 2014 |
referred to insurance |
Senate Bill S7103
2013-2014 Legislative Session
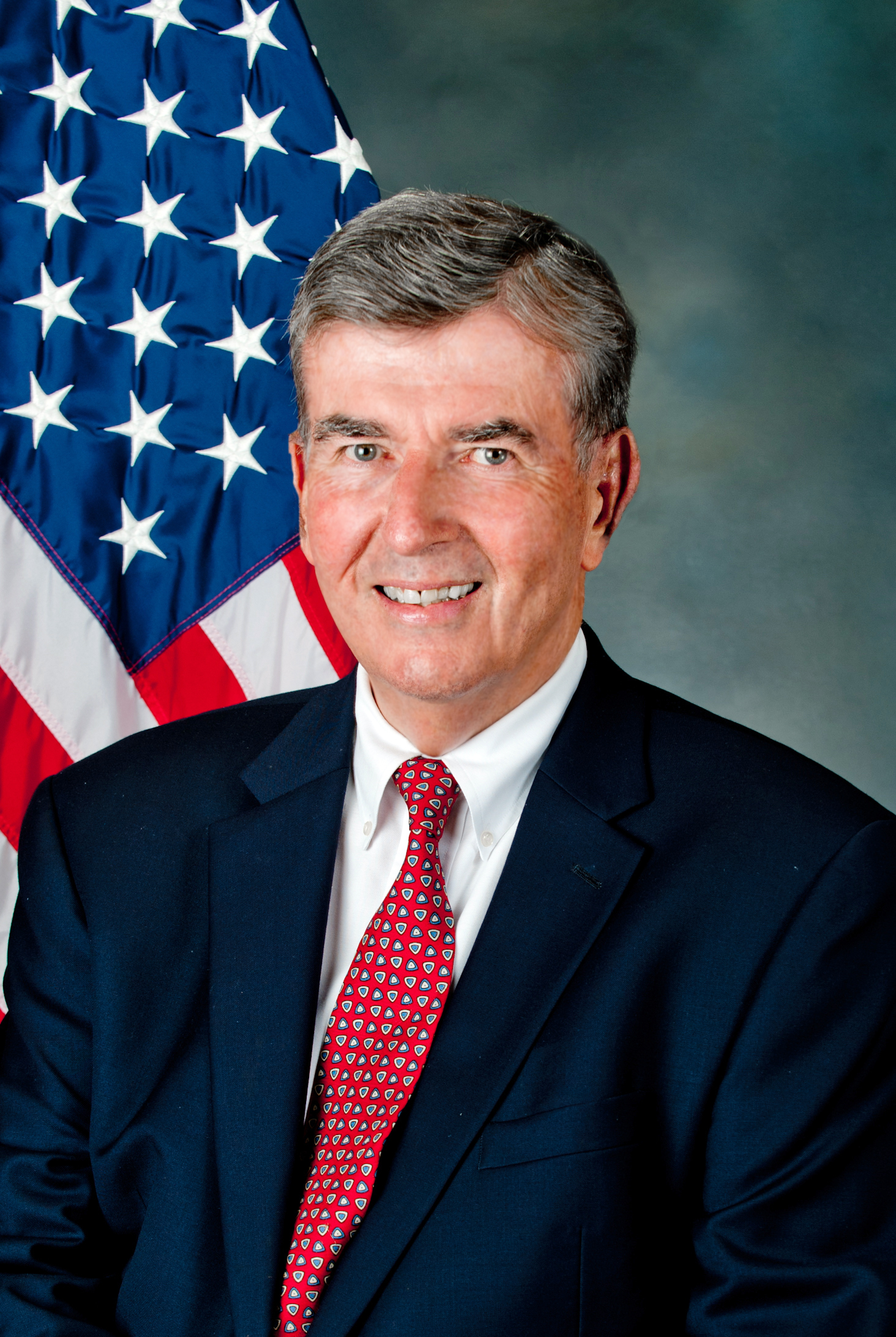
Sponsored By
(D) Senate District
Archive: Last Bill Status - In Senate Committee Insurance Committee
- Introduced
-
- In Committee Assembly
- In Committee Senate
-
- On Floor Calendar Assembly
- On Floor Calendar Senate
-
- Passed Assembly
- Passed Senate
- Delivered to Governor
- Signed By Governor
Actions
co-Sponsors
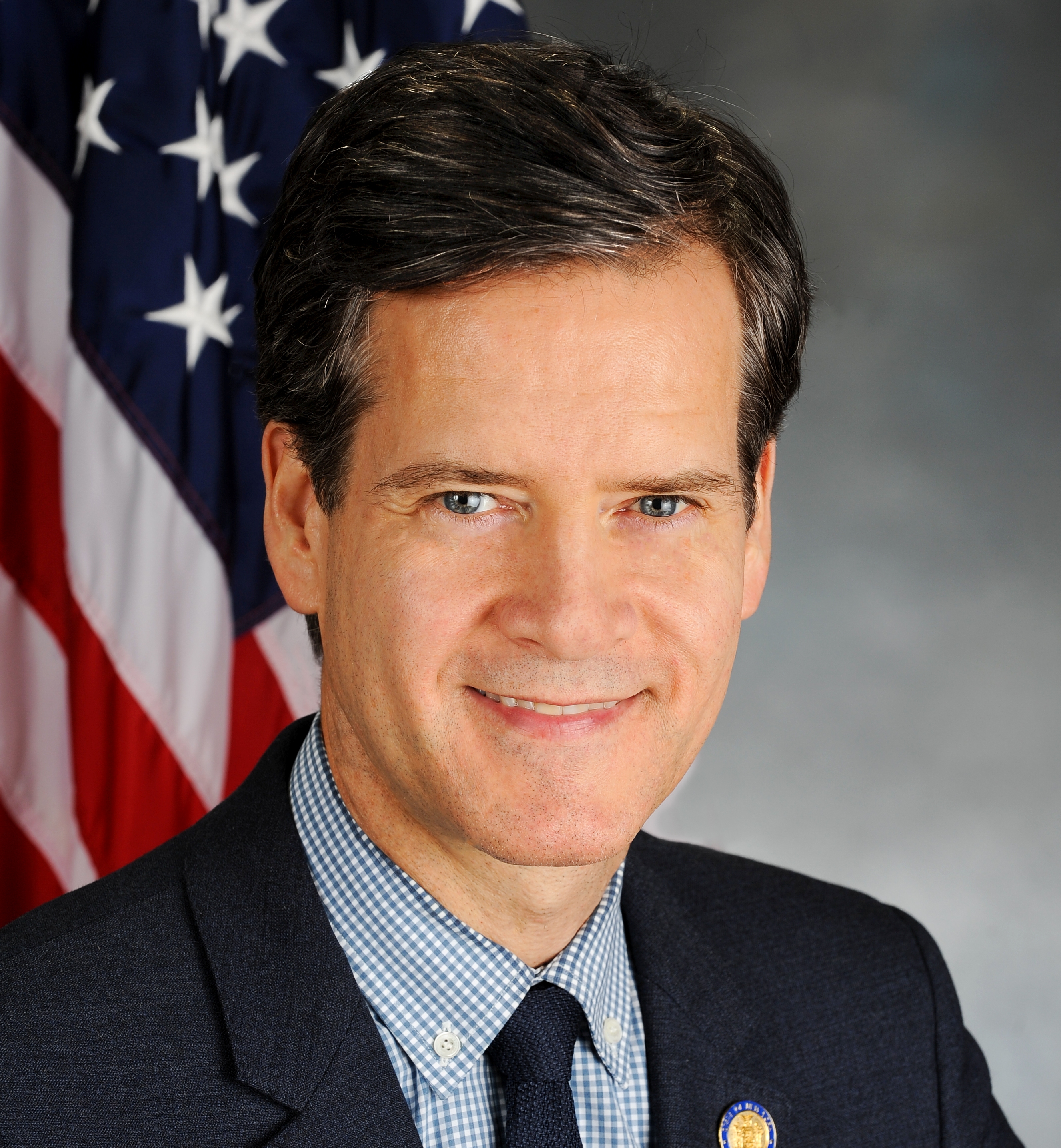
(D, WF) 46th Senate District
(D) Senate District
(D, WF) 47th Senate District
(D, WF) 28th Senate District
2013-S7103 (ACTIVE) - Details
- Current Committee:
- Senate Insurance
- Law Section:
- Insurance Law
- Laws Affected:
- Amd §§3216, 3221 & 4303, Ins L
2013-S7103 (ACTIVE) - Sponsor Memo
BILL NUMBER:S7103
TITLE OF BILL: An act to amend the insurance law, in relation to
requiring health insurance coverage for drug and alcohol abuse and
dependency treatment services
PURPOSE OR GENERAL IDEA OF BILL: To expand the time frame in which
insurance companies will provide coverage for rehabilitation of opioid
users.
SUMMARY OF SPECIFIC PROVISIONS: Section 1 amends subdivision B of para-
graph 30 of subsection (i) of section 3216 of the insurance law to
require every policy delivered or issued for delivery in New York State
increase the length of coverage for addiction rehabilitation to no less
than 60 days of treatment. It specifies that coverage can only be termi-
nated when the admitting or attending physician certifies that there is
no further treatment necessary and the patient should be discharged.
This allows for up to an additional 30 days of treatment, for a total of
90 days, if the admitting or attending physician deems it necessary.
It further provides that if the admitting or attending physician certi-
fies that treatment beyond 90 days is necessary, his or her certif-
ication shall be sufficient for eligibility for coverage through Medi-
caid as administered through county social services departments. Costs
associated with continued Medicaid coverage shall be borne by the state.
2013-S7103 (ACTIVE) - Bill Text download pdf
S T A T E O F N E W Y O R K
________________________________________________________________________
7103
I N S E N A T E
April 28, 2014
___________
Introduced by Sens. GIPSON, BRESLIN, DILAN, HOYLMAN, KRUEGER, PARKER,
PERKINS, STAVISKY -- read twice and ordered printed, and when printed
to be committed to the Committee on Insurance
AN ACT to amend the insurance law, in relation to requiring health
insurance coverage for drug and alcohol abuse and dependency treatment
services
THE PEOPLE OF THE STATE OF NEW YORK, REPRESENTED IN SENATE AND ASSEM-
BLY, DO ENACT AS FOLLOWS:
Section 1. Subsection (i) of section 3216 of the insurance law is
amended by adding a new paragraph 30 to read as follows:
(30) (A) EVERY POLICY DELIVERED OR ISSUED FOR DELIVERY IN THIS STATE
WHICH PROVIDES MEDICAL, MAJOR MEDICAL OR SIMILAR COMPREHENSIVE-TYPE
COVERAGE SHALL INCLUDE SPECIFIC COVERAGE FOR DRUG AND ALCOHOL ABUSE AND
DEPENDENCY TREATMENT SERVICES THAT ARE CERTIFIED AS NECESSARY BY A QUAL-
IFIED HEALTH PROFESSIONAL, AS DEFINED IN THE REGULATIONS OF THE COMMIS-
SIONER OF ALCOHOLISM AND SUBSTANCE ABUSE SERVICES.
(B) THE ONLY PREREQUISITE FOR THE COVERAGE OF HOSPITAL OR NON-HOSPITAL
BASED DETOXIFICATION, INCLUDING MEDICALLY MANAGED, MEDICALLY SUPERVISED
AND MEDICALLY MONITORED WITHDRAWAL, OR INPATIENT OR INTENSIVE RESIDEN-
TIAL REHABILITATION, OR INTENSIVE OR ROUTINE OUTPATIENT TREATMENT, SHALL
BE THAT A COVERED PERSON BE CERTIFIED AND REFERRED BY A QUALIFIED HEALTH
PROFESSIONAL. SUCH CERTIFICATION AND REFERRAL SHALL CONTROL BOTH THE
NATURE AND DURATION OF COVERED TREATMENT; PROVIDED, HOWEVER, THAT THE
DURATION OF SUCH COVERAGE SHALL NOT BE LESS THAN SIXTY DAYS AND MAY BE
TERMINATED ONLY WHEN AND IF THE ADMITTING OR ATTENDING PHYSICIAN, OR A
PHYSICIAN ASSISTANT OR NURSE PRACTITIONER ACTING UNDER THE SUPERVISION
OF THE ADMITTING OR ATTENDING PHYSICIAN, PROVIDING DETOXIFICATION, REHA-
BILITATION OR OUTPATIENT TREATMENT CERTIFIES THAT ADMISSION OF THE
COVERED PERSON IS NOT NECESSARY AND EARLY DISCHARGE IS APPROPRIATE. THE
DURATION OF SUCH COVERAGE SHALL BE EXTENDED BY AS MANY AS THIRTY ADDI-
TIONAL INPATIENT DAYS OR SESSIONS IF THE ADMITTING OR ATTENDING PHYSI-
CIAN, OR A PHYSICIAN ASSISTANT OR NURSE PRACTITIONER ACTING UNDER THE
SUPERVISION OF THE ADMITTING OR ATTENDING PHYSICIAN, DEEMS SUCH ADDI-
TIONAL DAYS OR SESSIONS ARE NECESSARY.
EXPLANATION--Matter in ITALICS (underscored) is new; matter in brackets
[ ] is old law to be omitted.
Comments
Open Legislation is a forum for New York State legislation. All comments are subject to review and community moderation is encouraged.
Comments deemed off-topic, commercial, campaign-related, self-promotional; or that contain profanity, hate or toxic speech; or that link to sites outside of the nysenate.gov domain are not permitted, and will not be published. Attempts to intimidate and silence contributors or deliberately deceive the public, including excessive or extraneous posting/posts, or coordinated activity, are prohibited and may result in the temporary or permanent banning of the user. Comment moderation is generally performed Monday through Friday. By contributing or voting you agree to the Terms of Participation and verify you are over 13.
Create an account. An account allows you to sign petitions with a single click, officially support or oppose key legislation, and follow issues, committees, and bills that matter to you. When you create an account, you agree to this platform's terms of participation.